Pelvic Torsion: Causes, Symptoms, and How to Correct It
- Updated - February 20, 2025
Pelvic torsion is a common yet often overlooked postural imbalance that can lead to chronic pain, movement dysfunction, and compensatory strain throughout the body.
Whether you are an athlete, a desk worker, or a healthcare professional, understanding pelvic torsion, why it occurs, and how to address it is crucial for pain relief and optimal movement.
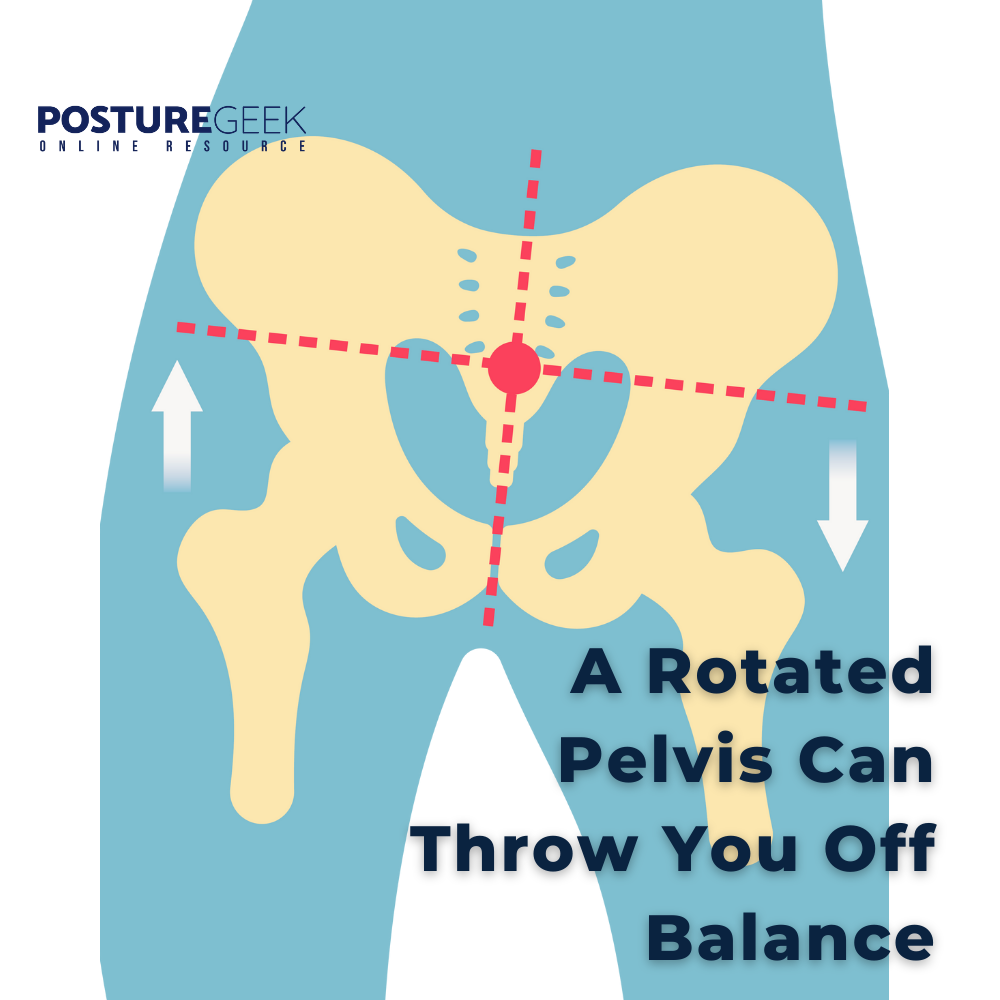
What Is Pelvic Torsion (Twisted Pelvis)?
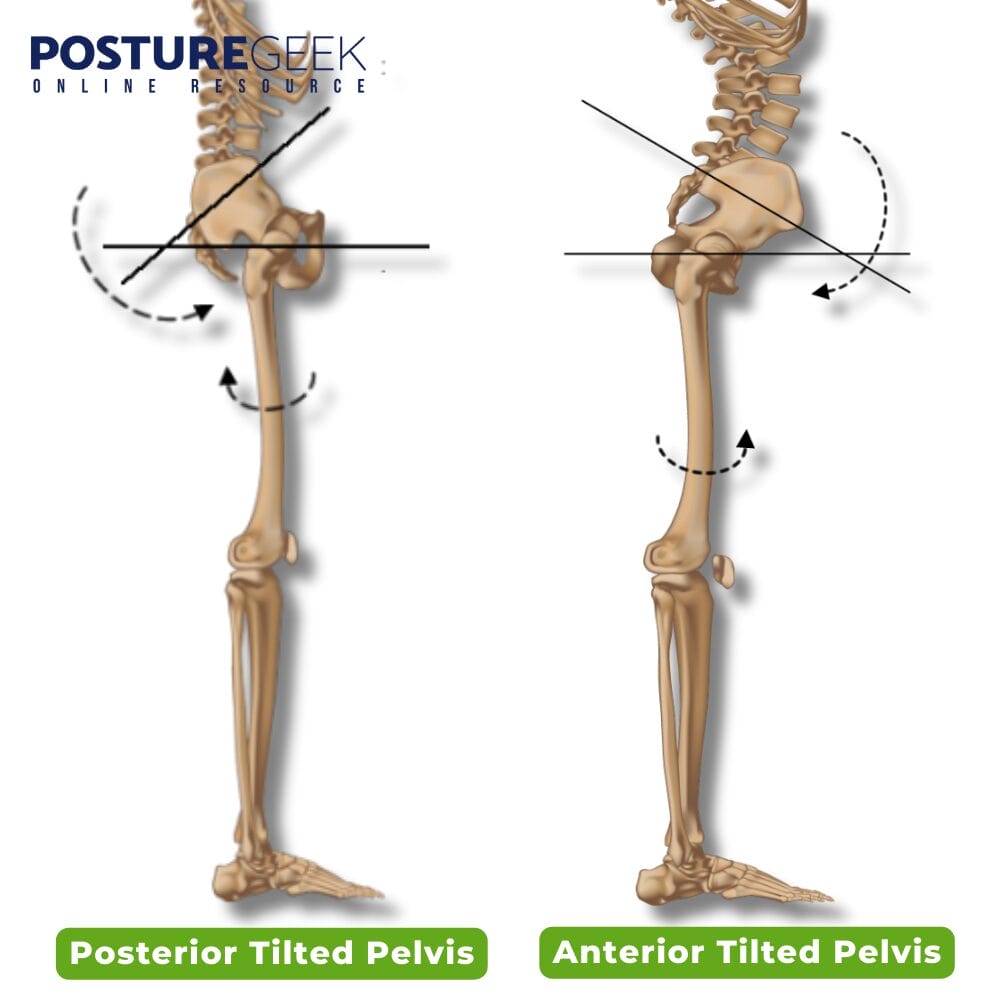
The pelvis is the body’s structural foundation, connecting the spine to the lower limbs and playing a central role in movement and stability. Ideally, the pelvis should be level and symmetrical, allowing for even weight distribution and efficient force transmission. However, when one side rotates forward (anterior pelvic tilt) or backward (posterior tilt) relative to the other, it results in pelvic torsion—a condition that disrupts alignment and function – and is sometimes described as a “twisted pelvis.”
How Pelvic Torsion Develops
The pelvis moves in three planes of motion:
- Sagittal plane (tilting forward and backward)
- Frontal plane (shifting side to side)
- Transverse plane (rotating left and right)
Under normal conditions, these movements allow the pelvis to adapt and stabilize during activities like walking, running, and squatting. However, muscle imbalances, particularly in the hip flexor muscles, movement dysfunctions, and postural habits can cause the pelvis to become stuck in a rotated position, leading to chronic misalignment.
Discover a practitioner near you.
Looking for a practitioner near you? Our extensive network of qualified professionals is here to help you.
Types of Pelvic Torsion
Pelvic torsion generally falls into two categories:
Anterior Pelvic Torsion (One side tilts forward)
- Increased lumbar curve (hyperlordosis)
- Tight hip flexors and quadriceps
- Weak glutes and hamstrings
- Common in athletes, dancers, and people who sit for long hours
Posterior Pelvic Torsion (One side tilts backward, also known as posterior pelvic rotation)
- Reduced lumbar curve (flattened lower back)
- Tight hamstrings and glutes
- Weak hip flexors and lower back muscles
- Often seen in individuals with habitual poor posture or previous injuries
What Causes Pelvic Torsion?
Pelvic torsion is not random—it results from long-term imbalances, habits, and structural adaptations leading to pelvic misalignment. Some of the most common contributors include:
Muscle Imbalances
- Tight hip flexors (psoas, rectus femoris) pull the pelvis forward, affecting the alignment of the hip bones.
- Tight hamstrings and glutes pull the pelvis backward.
- Weak core and obliques fail to stabilize pelvic positioning.
Leg Length Discrepancy & Pelvic Misalignment
A true or functional difference in leg length alters weight distribution, causing one side of the pelvis to rotate or drop lower, often due to anterior rotation.
A leg length discrepancy (LLD) occurs when one leg is structurally or functionally shorter, leading to uneven weight distribution and compensatory changes throughout the body.
Even a small difference in leg length can create asymmetry in the pelvis, spine, and lower extremities, contributing to pelvic torsion and postural misalignment.
Habitual Postures & Movement Patterns
- Sitting with one leg crossed over the other for extended periods.
- Standing asymmetrically, placing more weight on one hip.
- Standing with one hip higher than the other leads to lateral pelvic tilt.
- Repetitive sports movements like kicking, twisting, or running unevenly.
Trauma & Injury History
- Falls, car accidents, or impact injuries can shift the pelvis out of alignment.
- Dysfunction in the sacroiliac joints can create rotational asymmetry.
Foot & Gait Issues
- Overpronation (collapsed arch) or supination (high arch) affects pelvic stability.
- Scoliosis or spinal imbalances contribute to compensatory rotation of the pelvic bone.
Signs and Symptoms of Pelvic Torsion
Depending on its severity, pelvic torsion can present as mild discomfort or chronic pain. Some common symptoms include:
- Lower back pain (especially one-sided)
- Hip pain or tightness
- Sciatic-like symptoms (tingling or nerve pain)
- Uneven gait or difficulty walking
- One leg feels “longer” or “shorter” than the other
- Knee pain or foot pain due to altered weight distribution
If left unaddressed, pelvic torsion can lead to long-term compensations, including spinal misalignment, uneven muscle development, and chronic pain syndromes.
How Pelvic Torsion Affects Gait
Pelvic torsion doesn’t just impact posture—it has a direct influence on walking mechanics. Since the pelvis is the foundation of movement, any rotational imbalance can lead to uneven weight distribution, altered stride patterns, and compensatory muscle activation, which may contribute to discomfort or injury over time.
Uneven Hip Motion and Stride Length
In a neutral gait pattern, both hips move symmetrically in a forward and backward motion as you walk. However, when pelvic torsion is present:
- One side of the pelvis rotates forward (anterior torsion) while the other rotates backward (posterior torsion), disrupting the natural movement of the hips.
- This imbalance can cause one leg to extend further than the other, resulting in an uneven step pattern.
- Over time, the body compensates by adjusting stride length, which can lead to asymmetrical stress on the lower back, knees, and feet.
Leg Length Discrepancy and Weight Distribution
Pelvic torsion often creates a functional leg length discrepancy, making one leg appear longer than the other. This can cause:
- A compensatory limp or hip hike to clear the shorter leg.
- Increased load on one side of the body, leading to overuse injuries.
- Hip instability, which may result in SI joint irritation, tight glutes, or uneven lumbar strain.
Knee and Foot Mechanics Are Affected
Because the pelvis influences the entire kinetic chain, an imbalance at the pelvis can alter force absorption in the knees, ankles, and feet. This can lead to:
- Uneven pressure on the knees, increasing the risk of knee pain, patellar tracking issues, or meniscus strain.
- Foot imbalances, such as overpronation (collapsed arch) or excessive supination (rigid foot strike).
- A greater risk of ankle instability, plantar fasciitis, or Achilles tendon tension.
Changes in Arm Swing and Upper Body Movement
Walking is a full-body movement, requiring coordination between the pelvis, spine, and arms. Pelvic torsion can disrupt this rhythm, leading to:
- Asymmetrical arm swing, where one arm moves more than the other.
- Torso rotation imbalance, which may cause shoulder tension or neck discomfort.
- Increased energy expenditure due to inefficient movement patterns.
Recognizing Gait Alterations Due to Pelvic Torsion
If you suspect your gait is being affected by pelvic torsion, look for these signs:
- One foot lands harder or “slaps” the ground more than the other.
- The hip on one side hikes up or drops while walking.
- One step feels shorter or less stable than the other.
- Increased effort or fatigue in one leg compared to the other.
- Lower back or SI joint discomfort while walking.
Relationship between Pelvic Torsion and the Lumbar Spine
Pelvic torsion can profoundly impact the lumbar spine, often leading to lower back pain, stiffness, and restricted mobility. The lumbar spine is intricately connected to the pelvis, and any misalignment or rotation of the pelvic bones can disrupt the alignment and function of the lumbar spine.
The primary hip flexors, including the iliacus and psoas major, play a crucial role in maintaining the alignment and stability of the lumbar spine. When the pelvic bones are twisted or rotated, these hip flexors can create an imbalance. Some muscles may become overactive, while others may become underactive, leading to a cascade of issues.
This imbalance can manifest as lower back pain, stiffness, limited mobility, and challenging everyday activities. Addressing pelvic torsion is essential not only for pelvic health but also for the overall well-being of the lumbar spine and surrounding structures.
Diagnosing Pelvic Torsion

Diagnosing pelvic torsion requires a comprehensive hands-on assessment of the pelvic bones, lumbar spine, sacroiliac joints, and surrounding musculature. While imaging studies such as X-rays or MRIs may be used in some instances to rule out underlying structural issues, clinical evaluation remains the primary tool for identifying functional imbalances and asymmetries.
Clinical Assessment Strategies
Many healthcare professionals, including physical therapists, osteopaths, chiropractors, and manual therapists, use hands-on techniques to assess pelvic torsion, such as:
- Palpation of Bony Landmarks – Checking for asymmetry in the anterior superior iliac spine (ASIS), posterior superior iliac spine (PSIS), and sacral positioning.
- Leg Length Discrepancy Tests – Identifying whether pelvic torsion creates a functional short leg due to rotational imbalance.
- Standing and Supine Pelvic Assessments – Evaluating the alignment of the pelvis in different weight-bearing positions.
- Gait and Postural Analysis – Observing hip movement, stride length, and weight distribution during walking.
- Joint Mobility Tests – Checking sacroiliac joint movement and lumbar spine flexibility to detect restrictions.
- Muscle Strength and Imbalance Tests – Assessing the hip flexors, glutes, core, and lower back muscles for overactivity or weakness.
Key Clinical Findings
A diagnosis of pelvic torsion is typically based on a combination of physical signs and functional assessments, including:
- Abnormal pelvic alignment – One side of the pelvis may appear rotated forward or backward.
- Restricted lumbar or sacroiliac joint mobility – Stiffness or asymmetrical movement patterns.
- Muscle imbalances – Overactive hip flexors, weak glutes, or uneven tension in the hamstrings.
- Pain or tenderness – Localized discomfort in the pelvis, lower back, or sacroiliac joint.
- Asymmetrical movement patterns – Changes in gait, standing posture, or squat mechanics.
Why Clinical Diagnosis Matters
A hands-on clinical assessment allows practitioners to detect subtle movement dysfunctions that imaging may not reveal, making it a first-line diagnostic tool. Early identification through clinical evaluation enables targeted interventions, reducing the need for unnecessary imaging and ensuring effective treatment tailored to the individual’s unique postural and movement patterns.
By combining clinical expertise with movement-based assessments, healthcare professionals can develop a personalized treatment plan to restore pelvic balance, mobility, and function, preventing long-term complications.
How to Correct Pelvic Torsion

The good news is that pelvic torsion and associated pelvic discomfort can be addressed through a multifaceted approach combining manual therapy, targeted exercises, and postural awareness. By restoring balance to the pelvis, spine, and lower extremities, movement efficiency can improve, and pain can be reduced.
Manual Therapy & Hands-On Treatment
Various hands-on therapies can help release soft tissue restrictions, improve joint mobility, and restore proper pelvic alignment. Modalities that may assist include:
- Myofascial Release & Soft Tissue Therapy – Targets fascial restrictions that contribute to pelvic asymmetry.
- Chiropractic Adjustments & Osteopathic Manipulation – Realigns the sacroiliac joint, pelvic girdle, and lumbar spine.
- Massage Therapy & Neuromuscular Techniques – Loosens tight muscles, improves circulation, and enhances mobility.
- Physical Therapy & Manual Therapy Techniques – Addresses movement dysfunctions through hands-on mobilization and corrective exercises.
These therapies aim to correct imbalances, improve movement efficiency, and reduce strain on surrounding structures.
Corrective Exercises for Pelvic Alignment
Targeted exercises restore muscular balance by strengthening weak areas and improving flexibility where needed.
For Anterior Pelvic Torsion (Excessive Forward Tilt)
- Hip Flexor Stretch – Lengthens tight psoas and quadriceps, reducing the excessive pull on the pelvis.
- Glute Bridges – Strengthens the posterior chain (glutes, hamstrings) to counteract forward tilt.
- Deep Core Engagement (Dead Bug Exercise) – Activates transverse abdominis for pelvic stability.
For Posterior Pelvic Torsion & Posterior Pelvic Tilt
- Hamstring Stretches – Relieves excessive tension, pulling the pelvis backward.
- Hip Flexor Activation – Encourages better engagement of underactive hip flexors.
- Lumbar Extension Exercises – Strengthens lower back muscles for structural support.
These exercises should be performed consistently to reinforce postural correction and prevent recurrence.
Postural Awareness & Daily Habits
Many postural habits contribute to pelvic misalignment over time. Adjusting these day-to-day movements can help prevent or correct torsion.
- Avoid crossing your legs while sitting for extended periods.
- Distribute weight evenly when standing to avoid habitual shifting.
- Ensure ergonomic seating that supports neutral pelvic positioning.
- Be mindful of walking mechanics, avoiding excessive hip shifting or uneven gait patterns.
By making these adjustments, the body is given the opportunity to maintain better balance and function naturally.
Professional Assessment & Treatment
If pelvic torsion persists, seeking professional guidance can help pinpoint the root cause and provide a more tailored approach. Professionals who specialize in postural and movement correction include:
- Physical Therapists & Physiotherapists – Assess and treat movement dysfunctions affecting pelvic alignment.
- Osteopaths & Chiropractors – Work on joint mobility, spinal alignment, and muscular imbalances.
- Massage & Myofascial Therapists – Help release muscle tension and fascial restrictions affecting the pelvis.
- Movement Specialists (Pilates, Yoga, Feldenkrais Practitioners) – Guide individuals through movement retraining for better posture and coordination.
- Podiatrists & Orthotics Specialists – Address foot mechanics and gait abnormalities that may be influencing pelvic torsion.
By combining manual therapy, corrective exercise, postural awareness, and professional guidance, pelvic torsion can be effectively managed, reducing discomfort and improving functional movement.
Pelvic torsion is a multifaceted issue that requires an integrated approach to correction. Manual therapy, movement retraining, and postural adjustments restore balance and function. If you experience ongoing discomfort, working with a qualified professional can help determine the best course of action tailored to your specific needs.
Preventing Recurrence

Preventing the recurrence of pelvic torsion requires ongoing effort and attention to maintaining optimal alignment and function of the pelvic bones and lumbar spine. Regular exercise and stretching are vital to maintaining flexibility and strength in the primary hip flexors and surrounding muscles.
Maintaining good posture and avoiding repetitive strain or overuse can also help prevent recurrence. Ergonomic modifications in daily activities, such as using a supportive chair or taking regular breaks to stretch, can significantly reduce the risk of recurrence.
Regular check-ups with a healthcare professional can help identify any potential issues early on and prevent further complications. You can maintain pelvic health and overall well-being by staying proactive and attentive to your body’s needs.
Final Thoughts
Pelvic torsion is more than just a postural issue—it directly impacts movement efficiency, joint stability, and overall musculoskeletal health. Left unaddressed, it can lead to chronic pain, compensatory movement patterns, and long-term dysfunction affecting the lower back, hips, knees, and beyond.
The good news is that pelvic torsion is highly manageable with the right approach. By identifying the root causes—whether muscular imbalances, joint restrictions, or movement dysfunctions—you can apply targeted corrective strategies to restore pelvic alignment, improve posture, and enhance functional movement.
If you’re experiencing persistent discomfort, an uneven gait, or signs of postural misalignment, seeking guidance from a qualified professional can provide deeper insights and tailored interventions. Physical therapists, osteopaths, chiropractors, movement specialists, and myofascial therapists all bring unique expertise to help assess, treat, and guide you toward lasting balance and pain relief.
Taking proactive steps to address pelvic torsion today can prevent future complications, improve movement quality, and support a healthier, more resilient body. If you’re ready to take control of your posture and movement, start implementing these strategies and consult a professional who can help guide your journey toward optimal alignment and function.
Resources
Articles:
The Influence of Pelvic Tilt and Femoral Torsion on Hip Biomechanics: Implications for Clinical Assessment and Treatment
This comprehensive review examines how variations in pelvic tilt and femoral torsion significantly affect hip biomechanics, including acetabular orientation and range of motion. These alterations can lead to compensatory mechanisms impacting gait and posture.
- Read More Here
PLEASE NOTE
PostureGeek.com does not provide medical advice. This information is for educational purposes only and is not intended to be a substitute for professional medical attention. The information provided should not replace the advice and expertise of an accredited health care provider. Any inquiry into your care and any potential impact on your health and wellbeing should be directed to your health care provider. All information is for educational purposes only and is not intended to be a substitute for professional medical care or treatment.
About the author
Join our conversation online and stay updated with our latest articles.
Find Expert Posture Practitioner Near You
Discover our Posture Focused Practitioner Directory, tailored to connect you with local experts committed to Improving Balance, Reducing Pain, and Enhancing Mobility.