Understanding Metatarsalgia
A Global Perspective on a Local Foot Pain Problem
- Updated - June 16, 2025
Metatarsalgia may begin as a minor irritation in the ball of your foot, but its effects can significantly impact the way you walk, stand, and move.
Metatarsalgia is considered a common overuse injury, especially among active individuals or those exposed to repetitive stress, such as athletes in high-impact sports.
While the pain is often focused on the ball of the foot, the cause and impact extend far beyond. In some cases, metatarsalgia can lead to widespread pain, affecting larger areas of the foot or even the middle of the foot, particularly in those involved in high-impact activities or with inflammatory conditions.

What Is Metatarsalgia?
Metatarsalgia refers to pain and inflammation in the ball of the foot, typically located under the second to fourth metatarsal heads.
Primary metatarsalgia refers to pain caused by issues within the metatarsal bones themselves, affecting their interaction with surrounding foot structures.
Metatarsalgia can cause sensations ranging from sharp and shooting to aching and burning. It is not a diagnosis but a symptom that results from various underlying biomechanical or structural issues.
Common Symptoms:
- A burning pain or aching pain in the forefoot
- The sensation of standing on a small stone or lump
- Increased discomfort when walking barefoot or during push-off
- Shooting pain in the ball of your foot
Understanding the Anatomy of the Foot
To fully grasp metatarsalgia, it helps to understand the architecture of the forefoot and how its structures interact under load. The foot serves as both a shock absorber and a propulsion engine, handling complex forces every time we move.
Discover a practitioner near you.
Looking for a practitioner near you? Our extensive network of qualified professionals is here to help you.
Key Structures Involved in Metatarsalgia: Focus on the Ball of the Foot
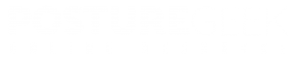
- Metatarsal Bones
- The forefoot contains five metatarsal bones that connect the midfoot to the toes.
- Pain typically centers at the second to fourth metatarsal heads, which bear the brunt of load during the toe-off phase of gait.
- A long second metatarsal or uneven weight distribution often makes this region more vulnerable.
- Plantar Plate and Ligaments
- The plantar plate is a fibrous structure that stabilizes the base of the toes and anchors the metatarsophalangeal joints.
- Repetitive strain or breakdown of this structure can lead to severe pain, instability, or toe deformities like hammer toes.
- Intermetatarsal Bursae
- These small fluid-filled sacs reduce friction between metatarsal bones.
- When irritated due to compression or overload, they can become inflamed, contributing to pain.
- Intrinsic Foot Muscles
- Muscles such as the lumbrical and interossei muscles of the foot help maintain toe alignment and foot stability.
- Weakness in these muscles shifts stress to passive structures, such as ligaments and fat pads.
- Fat Pad Cushioning
- A natural fat pad under the metatarsal heads acts as a shock absorber.
- With age or repeated high-impact activity, this pad can thin or migrate, leaving bones more exposed to ground forces.
- The plantar fascia connects the heel to the toes and plays a role in arch integrity.
- Fascial restrictions can pull on the forefoot, subtly altering load mechanics and increasing stress on the metatarsals.
By understanding the anatomy and how these structures function together, practitioners can better identify the causes of symptoms and how to address them both locally and systemically. This also reinforces the need to move beyond symptom treatment and explore how alignment, stability, and movement patterns influence forefoot health.
What Triggers Metatarsalgia?
The condition can develop due to a combination of local overload and systemic issues. Triggers may include:
- High-impact sports or repetitive forefoot loading
- Footwear with inadequate arch support, narrow toe boxes, high heels, or tight, pointy shoes
- Long second metatarsal or uneven metatarsal length
- High arch or flat feet
- Reduced fat pad cushioning under the ball of the foot
- Medical conditions like rheumatoid arthritis or diabetes
- Postural compensations or poor gait mechanics
- Activities performed on a hard surface, such as concrete or hardwood floors
The primary risk factors for metatarsalgia include participation in high-impact sports, wearing high-heeled shoes, and having foot deformities.
Understanding the trigger is crucial for identifying the appropriate intervention. Excessive pressure or prolonged pressure on the forefoot, often caused by ill-fitting shoes or high-impact activities, can lead to the development of metatarsalgia.
Will Metatarsalgia Go Away?
Metatarsalgia can be resolved, but only if the contributing factors are identified and addressed. If left untreated or managed solely at the site of pain, it may become a chronic issue. However, with proper load management, footwear changes, and biomechanical support, most cases can improve significantly.
Achieving pain relief is an important goal during recovery, alongside addressing the underlying contributing factors. Over-the-counter medications and other conservative treatments are often effective for mild to moderate pain.
Recovery Factors:
- Early intervention
- Reducing aggravating activities
- Correcting biomechanical contributors
- Integrative treatment targeting both local and global function
Local Pain, Global Impact
Metatarsalgia may begin as a localized irritation in the ball of the foot, but its influence rarely stays confined to that region.
The human body is built to adapt, and when a key structure, such as the forefoot, becomes painful or dysfunctional, the entire kinetic chain responds. These adaptations often go unnoticed at first, but over time, they can create a cascade of compensatory patterns, leading to broader discomfort, poor performance, and chronic strain.
Why Local Pain Affects the Whole System
The foot plays a central role in both stability and movement. It’s the first point of contact with the ground during walking and running, and its ability to absorb shock, adapt to surfaces, and transfer force upward is essential for healthy locomotion.
When pain alters how the foot loads or pushes off, the rest of the body must adjust to maintain balance, momentum, and functional movement. These adjustments can result in misalignments, overuse, or inefficient motor patterns elsewhere in the system.
Common Global Consequences of Metatarsalgia
- Altered Gait Mechanics
To avoid pain during walking, people often modify their stride unconsciously. This might involve shortening steps, reducing push-off force, or shifting pressure to the lateral foot or heel. These changes disrupt normal gait cycles and place abnormal stress on surrounding joints.
- Postural Compensation
As load shifts away from the forefoot, compensatory patterns can develop in the lower limb and spine. A person may externally rotate the hips, lean backward slightly, or lock the knees during stance. These subtle shifts can alter the alignment of the knees, hips, pelvis, and even the thoracic spine, all key components influenced by the posterior chain.
- Core and Pelvic Instability
The feet influence how force is transferred up to the pelvis and trunk. When the forefoot is offloading improperly, the pelvic stabilizers may become underused or overactive. Over time, this imbalance can contribute to reduced core activation, sacroiliac discomfort, and altered pelvic tilt.
- Decreased Movement Efficiency
Whether walking, running, or simply standing, every compensatory adjustment costs energy. The result is reduced mechanical efficiency, quicker fatigue, and diminished performance. In clinical terms, clients may describe feeling “off,” unstable, or restricted in movement even though the original issue is located in the foot.
- Secondary Overuse Injuries
The longer these compensations persist, the greater the risk for overuse injuries in regions that were not initially involved. Common secondary issues may include:
- Iliotibial band syndrome
- Patellofemoral pain
- Hip bursitis
- Low back tightness or strain
Plantar fasciitis or Achilles tendinopathy (from poor offloading strategies)
Why Health Care Professionals Must Look Beyond the Foot
Treating the site of pain alone often results in only short-term relief. A foot-focused intervention, while necessary, must be paired with global assessment and correction strategies. This includes addressing movement quality, restoring load balance across both feet, and re-establishing efficient gait and posture through strength, mobility, and neuromuscular control.
What Exercises Should You Avoid with Metatarsalgia?

Specific exercises can aggravate the condition, especially those that increase pressure through the forefoot or rely on unstable foot positioning.
Avoid:
- High-impact jumping or bounding activities
- Barefoot running, especially on hard surfaces
- Exercises that require prolonged forefoot loading, like deep lunges or certain yoga poses
- Plyometric drills on hard or uneven surfaces
Instead, focus on exercises that build foot strength, improve mobility, and encourage full-foot loading without excessive pressure at the metatarsal heads.
Assessment Matters: Local and Global

Effective care begins with a clear and thorough assessment that considers both the pain site and the broader movement system.
Local Assessment:
- Palpation of the metatarsal heads, including assessment of the surrounding soft tissues for signs of inflammation or injury
- Observation of callus patterns or digital deformities
- Range of motion in toes and arches
- Load distribution during stance and gait
Global Assessment:
- Gait analysis focusing on push-off and stride length.
- Hip, knee, and pelvis alignment under load.
- Core engagement and posture during movement.
- Functional tests such as single-leg stance, squats, or step-downs.
How Do You Treat Metatarsalgia?
Metatarsalgia rarely resolves with isolated or surface-level interventions.
To achieve meaningful and lasting results, treatment must address both the symptomatic relief at the forefoot and the underlying biomechanical patterns that caused the overload.
Successful care involves a combination of targeted local strategies and broader movement correction—often across multiple sessions.
Local Interventions for Metatarsalgia Pain Relief
These strategies focus on reducing stress at the metatarsal heads, improving foot biomechanics, and addressing tissue irritation.
Footwear Adjustments
- Select shoes with wide toe boxes, sufficient forefoot cushioning, and sturdy soles to minimize excessive bending. It is important to wear shoes that fit well and provide proper arch support. Avoid high heels and narrow, tapered shoes that compress the forefoot and big toe, as wearing high heels can increase stress on the foot and worsen pain.
Metatarsal Pads or Custom Orthotics
- Properly placed metatarsal pads lift and offload the metatarsal heads, redistributing pressure more evenly. In cases of structural issues, such as a long second metatarsal, custom orthotics can help restore mechanical balance during walking and running.
Manual Therapy Techniques
- Releasing tight or overworked muscles, such as the toe extensors, plantar fascia, or peroneal muscles, can help reduce tension through the forefoot. Techniques may include myofascial release, joint mobilizations, or trigger point therapy.
Supportive Taping Methods
- Taping techniques can offer temporary relief by lifting tissue, reducing ground contact pressure, and encouraging correct toe alignment. This can also improve proprioception and load awareness during movement.
Targeted Strengthening for Intrinsics
- Rebuilding the function of the small muscles within the foot improves load distribution, stability, and resilience. Exercises like toe spreading, doming (short foot), and towel scrunches help restore muscular control at the source of the problem.
Ice Pack Application
- Applying an ice pack directly to the affected area for short periods can help reduce pain and inflammation in the foot.
Global Interventions for Root-Cause Correction
To prevent recurrence and support full-body integration, practitioners should address postural control, gait efficiency, and motor coordination across the lower kinetic chain.
Hip and Core Strengthening
- Weakness in the glutes, especially the glute medius, and rotators, can shift loading into the forefoot during stance. Core instability also leads to poor pelvic control, which affects how weight is transferred through the legs and feet.
Gait Retraining
- Many individuals with metatarsalgia develop habits such as toe gripping, a shortened stride, or excessive midfoot loading. Gait retraining can restore proper heel-to-toe mechanics and reintroduce full-foot loading, especially during terminal stance and push-off.
Mobility Restoration for Ankles and Hips
- Limitations in ankle dorsiflexion or hip extension often force compensation at the foot. Addressing these restrictions through active mobility drills, soft tissue release, and dynamic stretching helps free up the kinetic chain and improves loading patterns.
Neuromuscular Re-Patterning
- Chronic forefoot pain often leads to poor foot-ground interaction and delayed muscular responses. Proprioceptive work, including balance tools, barefoot ground drills, and sensory feedback training, can help re-establish coordinated foot engagement and improve control under load.
Additional Considerations
Education and Load Management
- Clients should be educated on activity modification, pacing, and recognizing early signs of overload. This empowers them to take responsibility for their recovery while reducing flare-ups.
Addressing Movement Habits
- Long-standing compensations won’t resolve overnight. Patterns such as overstriding, toe gripping, or lateral foot dominance may require weeks of intentional retraining with guided support.
Cross-Training and Recovery Practices
- Low-impact activities, such as swimming, cycling, or using an anti-gravity treadmill, can help maintain fitness while offloading pressure from the forefoot. Restorative practices such as contrast baths or compression therapy may also support tissue recovery.
In summary, the most effective treatment plan for metatarsalgia is not just about relieving pain in the foot but about building a more resilient and balanced system that moves efficiently. Addressing the forefoot, while essential, is only one piece of the puzzle.
Final Thoughts: A Whole-Person Approach
Metatarsalgia may present as foot pain, but it often reveals larger issues in load management, gait control, and systemic movement efficiency. Focusing only on symptom relief without addressing the entire chain of movement sets the stage for recurrence.
To truly resolve metatarsalgia:
- Look beyond the foot and explore the root causes
- Educate clients about load, alignment, and movement awareness
- Address both local irritation and global dysfunction
Support with a mix of manual therapy, corrective exercise, and behavior change
If you’re a practitioner seeking deeper tools for assessing and resolving conditions like metatarsalgia, the Integrated Posture Assessment Framework (IPAF) course offers a modern, structured approach to movement health that moves beyond surface-level symptoms.
Resources
Articles:
Impact of Different Foot Orthoses on Gait Biomechanics in Individuals with Chronic Metatarsalgia
- Published: 2025
- Summary: This study examines how various foot orthoses affect gait biomechanics in individuals suffering from chronic metatarsalgia. It highlights the importance of personalized orthotic interventions in alleviating pain and improving walking patterns.
- Read Article
PLEASE NOTE
PostureGeek.com does not provide medical advice. This information is for educational purposes only and is not intended to be a substitute for professional medical attention. The information provided should not replace the advice and expertise of an accredited health care provider. Any inquiry into your care and any potential impact on your health and wellbeing should be directed to your health care provider. All information is for educational purposes only and is not intended to be a substitute for professional medical care or treatment.
About the author
Join our conversation online and stay updated with our latest articles.
Find Expert Posture Practitioner Near You
Discover our Posture Focused Practitioner Directory, tailored to connect you with local experts committed to Improving Balance, Reducing Pain, and Enhancing Mobility.